Abstract
Introduction Cytogenetic abnormalities (CA) identified by interphase fluorescence in situ hybridization (iFISH) has been served as the cornerstone for risk stratification at diagnosis. However, iFISH analyses were generally performed in newly diagnosed and relapsed multiple myeloma (MM) patients, but CA architecture has received little attention in patients after induction therapy. Since it is not the be-all and end-all for everyone to achieve minimal residual disease (MRD)-negativity. iFISH assay may be a good tool to explore the nature of residual plasma cells (PCs) and has proven to be a reliable complementary technique for MRD detection. We thus performed iFISH analyses after proteasome inhibitor (PI) or immunomodulatory drugs (IMiDs) induction in our prospective clinical trial.
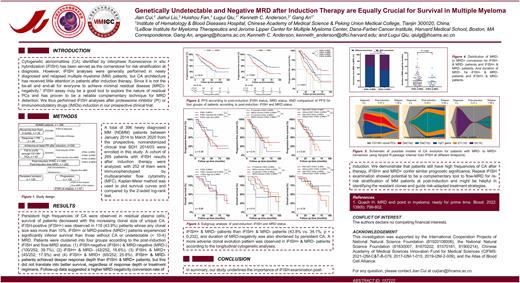
Methods A total of 396 patients with NDMM between January 2014 and March 2020 who had cytogenetic analysis by iFISH both at diagnosis and within 6 months from the start of induction therapy were included in this study. All of the participants in this study were enrolled in the prospective, non-randomized clinical trial (BDH 2014/03), which was a part of the National Longitudinal Cohort of Hematological Diseases in China (NCT04645199). A cohort of 269 patients with iFISH results after induction therapy were analyzed, with 252 of them were immunophenotyped by multiparameter flow cytometry. The median follow-up time was 41.5 months (25th/75th, 26.5/61.4 months) for the 269 patients who underwent post-induction iFISH analyses. Kaplan-Meier method was used to plot survival curves and compared by the 2-sided log-rank test. We also investigated the interaction between post-induction flow-MRD and iFISH status concerning patient outcomes. Multivariable Cox proportional hazard regression was used to assess the impact of variables on PFS and OS.
Results Persistent high frequencies of CA were observed in residual PCs, survival of patients decreased with the increasing clonal size of unique CA. iFISH-positive (iFISH+) was observed in 118 (43.9%) patients whose any clonal size was more than 10%. FISH-positive patients or MRD-positive (MRD+) patients experienced significantly inferior survival than those without CA or undetectable (< 10-4) MRD. Patients were clustered into four groups according to the iFISH and flow-MRD status: (1) iFISH-negative (iFISH-) & MRD-negative (MRD-) (100/252, 39.7%), (2) iFISH+ & MRD- (42/252, 16.6%), (3) iFISH- & MRD+ (45/252, 17.9%) and (4) iFISH+ & MRD+ (65/252, 25.8%). iFISH+ & MRD- patients achieved deeper response depth than iFISH- & MRD+ patients, but this did not translate into better survival, regardless of response depth or treatment regimens. An adjusted survival analysis was performed and showed that the survival outcomes of the 4 clusters in the adjusted analysis and the crude analysis were identical, and that outcomes were similar between patients with iFISH+ & MRD- and those with iFISH- & MRD+ (mPFS: 49.49 months vs. 41.49 months; mOS: 75.33 vs. 70.74 months). Follow-up suggested that persistent CA in residual PCs facilitated the conversion of MRD- to MRD+. The MRD- conversion rate was slightly higher in patients with iFISH+ & MRD- than iFISH- & MRD- (49% vs. 36%, p = 0.139), and the duration of MRD- was also shortened by persistent CA. Longitudinal iFISH examinations were available for 21 patients with MRD- conversion at 3 time points: at diagnosis, post-induction, and at relapse. Notably, a more adverse clonal evolution pattern was observed among patients with iFISH+ & MRD-, with 5 cases of linear evolution at relapse.
Conclusions In summary, our study underscores the importance of tumor cell biological characteristics examinations post-induction among patients with NDMM. We demonstrated that patients continued to have high frequencies of CA after therapy. iFISH examination after induction therapy not only provided a complementary tool to flow-MRD but also deciphered the cytogenetic profiles of residual PCs based on the quantification of these residual PCs. This comprehensive approach of combining flow-MRD and iFISH examination leverages common tests. Therefore, it may be practical to adapt in clinical practice to help identify the resistant clones and guide risk-adapted treatment strategies.
Disclosures
Anderson:Precision Biosciences: Membership on an entity's Board of Directors or advisory committees; Raqia: Other: Scientific founder ; C4 Therapeutics: Other: Scientific founder ; Starton: Membership on an entity's Board of Directors or advisory committees; NextRNA: Other: Scientific founder ; Janssen: Membership on an entity's Board of Directors or advisory committees; AstraZeneca: Membership on an entity's Board of Directors or advisory committees; Amgen: Membership on an entity's Board of Directors or advisory committees; Dynamic Cell Therapy: Current holder of stock options in a privately-held company, Membership on an entity's Board of Directors or advisory committees; Mana Therapeutics: Membership on an entity's Board of Directors or advisory committees; OncoPep: Other: Scientific founder ; Window: Membership on an entity's Board of Directors or advisory committees; Pfizer: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal